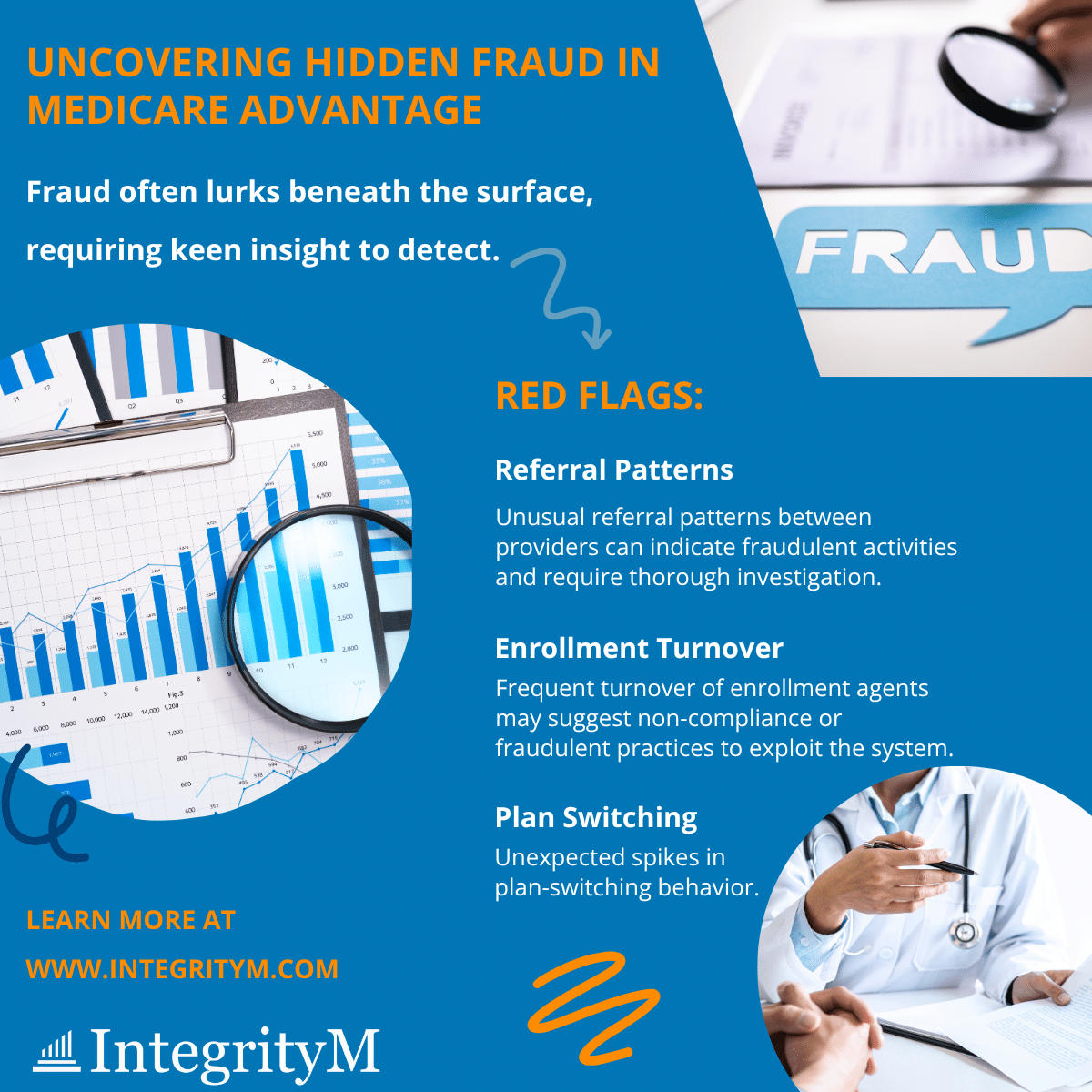
To uphold program integrity, look beyond obvious data anomalies and consider these critical warning signs:
- Unusual referral patterns between providers/suppliers
- Frequent turnover of enrollment agents
- Unexpected spikes in plan-switching behavior
At IntegrityM, we recognize that effective fraud detection requires both expertise and nuance. Our specialized approach combines advanced data analytics, comprehensive audits, and expert medical reviews to uncover complex fraud, waste, and abuse schemes that others might miss.
We’re dedicated to protecting vulnerable beneficiaries and preserving the Medicare Trust Funds for future generations.
Remember: Fraud isn’t always blatant, but patterns speak.
Learn more and join us in shaping the future of healthcare integrity: Contact IntegrityM











